Team Leaders: Dr. Chad Perlyn, M.D. and Shannon Del Prado
Team Type: Plastic Surgery
Campaign Summary:
We triaged 68 patients. We did 27 major operations under general anesthesia and another 24 under local anesthesia.
The major operations included cleft lips, cleft palates, burn scar releases, lipoma removals, and hand surgeries. The procedures under local anesthesia were lesion removals and scar revisions.
Supporters:
Friends of Project Peru – Miami, Florida
Mike and Judith Rizo – Cooper City, Florida
Team Members and Roles:
Anonymous
Leonard Aguero, R.N.
Lucia Burga, Photographer
Dr. Cathy Burnweit, M.D., Pediatric General Surgeon
Marlene Cueller, R.N.
Shannon Del Prado, Co-leader
Dr. Ashley Ehret, M.D., Surgeon
Dr. Rafael Gonzalez, M.D., Anesthesiologist
Hoah Heredia, Surgical Technician
Anna Pelligra, Nurse Practitioner
Jose Perdomo, R.N.
Nancy Perdomo, R.N.
Brooke Perlyn, Assistant
Dr. Chad Perlyn, M.D., Plastic Surgeon
Stanley Pierre, C.R.N.A.
Cassandra Pita, Assistant
Howard Pita, Assistant
Lucian Kraft Pita, Assistant
Rose Richemond, C.R.N.A.
Judith Rizo, Pharmacist
Mike Rizo, Pharmacist
Amie Roberts, R.N.
Noraisy Rodriguez, R.N.
Elizabeth Roman, R.N.
Mia Schatz, Medical Scribe
Camila Suarez, Assistant
General Narrative:
By Dr. Chad Perlyn, M.D.
Our July 2024 medical mission to Peru was a powerful demonstration of compassionate care, surgical excellence, and interdisciplinary collaboration. Over the course of the trip, we provided critical surgical interventions to both pediatric and adult patients in a region with limited access to specialized care.
We performed surgeries on numerous children suffering from burn injuries, cleft lip and palate deformities, and complex congenital conditions. Additionally, we treated adult patients with large tumors and other serious health concerns, many of whom had been waiting months or years for care.
One of the most extraordinary cases involved a young boy who was transferred to us in the middle of the night from a nearby hospital after suffering devastating facial trauma that included multiple fractures and the near-complete avulsion of his upper lip. Thanks to the swift response and expertise of our team, we were able to operate urgently and successfully—reconstructing his face and saving his upper lip.
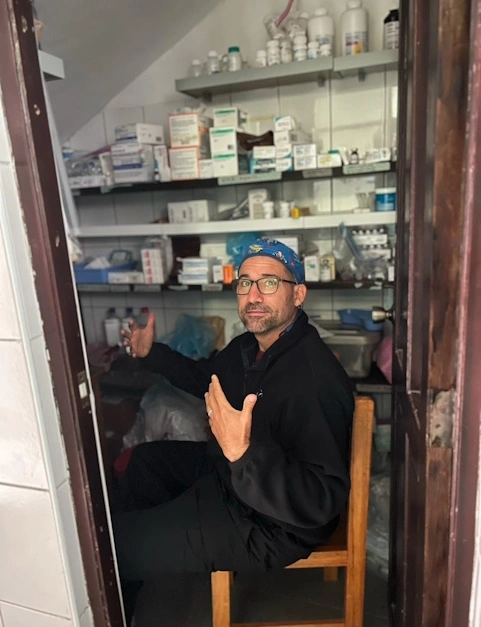
Beyond surgical care, our mission also focused on sustainability and systems strengthening. We reorganized the hospital pharmacy, resupplied critical surgical materials, and addressed several longstanding inventory and logistics challenges.
Finally, we prioritized capacity-building through education, conducting hands-on training sessions and surgical workshops for local healthcare staff. These efforts aimed to leave behind not just healthier patients, but also a stronger, more equipped healthcare team.
This mission was a testament to what can be accomplished when skill, purpose, and service come together. We are grateful to the local teams, the community, and all those who made this work possible.
Narrative Supplement About the Twelve Year Old Child
By Dr. Chad Perlyn, M.D.
DTRT: Do the Right Thing These four letters have guided many of my decisions, including a recent one in Peru. We had a team of 24 pediatric surgical professionals, many from Nicklaus Children’s Health System, working with our Peruvian colleagues in the Andes. After several intense days, we went to another town for a break and group dinner. As the celebration began, a Peruvian nurse called out “Dr. Chad,” showing me a photo of a 12-year-old boy injured in a bicycle accident. His upper lip was almost completely ripped off, his nose crushed, teeth broken, eye swollen, and face lacerated. The nurse said he was at a local hospital but needed care they couldn’t provide and would be transferred to a big city, which would take a day. She knew that his lip would not survive and said they had a pick-up truck ready to bring him to us. Just as our dinner started, I announced we needed to go to work.
We headed back to Kausay Wasi and prepared the tiny operating room. The fear on the father’s face when they arrived was unforgettable. Sobbing, he begged us in Quechuan to take care of his boy. “I have two sons of my own, but know that I will have three children tonight,” I told him through our translator. Within minutes, our team validated the trauma assessment and our anesthesiologists safely put the boy to sleep using rapid sequence induction. My colleague, plastic surgeon Dr. Ashley Ehret, joined me in the operating room. Ashley’s brilliant idea to replicate how leeches drain blood worked, and the dark swollen lip began to show signs of life.
It was past midnight when we finished. We looked up to see the team, both U.S. and Peruvian, supporting us. As we brought the child out of the operating room, our incredible team of APRNs, nurses, and pharmacists ensured his safety and comfort as he woke up.
A few days later, Dr. Ashley and I took a photo with his mother. Though her gratitude was spoken in Quechuan, her smile and hug said it all. As I head to the airport, I reflect on why I shared this. Yes, it’s a beautiful photo and story, but there’s a deeper hope. Medicine is changing. As a senior leader in healthcare, I see this every day—from metrics to relative value units (RVUs), contract negotiations, space shortages, competition, and payment cuts. I share this story with the hope that our future doctors, nurses, pharmacists, and others going into healthcare remember this: Nothing about the essence of medicine has changed. Since the beginning of humanity, some of us have chosen a life of service to heal the injured or sick. The ability to help another person is the most powerful asset you will have. Treasure it. None of us can change healthcare delivery alone, but we can decide how we will deliver that care. One day, you too will get calls to help. Some will be mundane, some complex, some at home, some away. What matters is remembering who we are as a profession when you answer that call and why you went into medicine. DTRT.